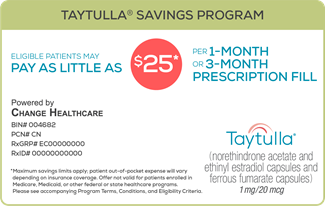
Taytulla® Patient Savings Program Terms
Program Terms, Conditions, and Eligibility Criteria:
- This offer is available to patients with commercial prescription insurance coverage and a valid prescription of Taytulla® (norethindrone acetate and ethinyl estradiol capsules and ferrous fumarate capsules) at the time the prescription is filled by the pharmacist and dispensed to the patient.
- Depending on your insurance coverage, most eligible patients may pay as little as $25 for each of up to thirteen (13) prescription fills of a 28-day supply OR each of up to four (4) prescription fills of an 84-day supply. Check with your pharmacist for your copay discount. Maximum savings limits apply; patient out-of-pocket expense will vary.
- This card is not valid for use by patients enrolled in Medicare, Medicaid, or other federal or state programs (including any state pharmaceutical assistance programs), or private indemnity or HMO insurance plans that reimburse you for the entire cost of your prescription drugs. Patients may not use this card if they are Medicare-eligible and enrolled in an employer-sponsored health plan or prescription drug benefit program for retirees. This offer is not valid for cash-paying patients.
- AbbVie reserves the right to rescind, revoke, or amend this offer without notice.
- Offer good only in the USA, including Puerto Rico, at participating retail pharmacies.
- Void if prohibited by law, taxed, or restricted.
- This card is not transferable. The selling, purchasing, trading, or counterfeiting of this card is prohibited by law.
- This card has no cash value and may not be used in combination with any other discount, coupon, rebate, free trial, or similar offer for the specified prescription.
- This offer is not health insurance.
- Subject to all other terms and conditions, the maximum annual benefit that may be available solely for the patient’s benefit under the copay assistance program is $2,220 per calendar year. The actual application and use of the benefit available under the copay assistance program may vary on a monthly, quarterly, and/or annual basis depending on each individual patient’s plan of insurance and other prescription drug costs.
- By redeeming this card, you acknowledge that you are an eligible patient and that you understand and agree to comply with the terms and conditions of this offer.
To learn about AbbVie’s privacy practices and your privacy choices,
visit www.abbvie.com/privacy.html.
If you are a patient and have questions about the program, including savings on mail-order prescriptions,
please call 1.855.439.2817.